Up to 80% of people will experience back pain at some point in their lives, and herniated discs are frequently the culprit. This problem can cause intense discomfort. Imagine a jelly-filled doughnut squishing out its filling, and you have a rudimentary idea of what’s happening.
Discs absorb shocks between the vertebrae in your spine. However, when they herniate, they can press on nearby nerves, causing a spectrum of symptoms that range from dull aches to debilitating pain, tingling and even muscle weakness.
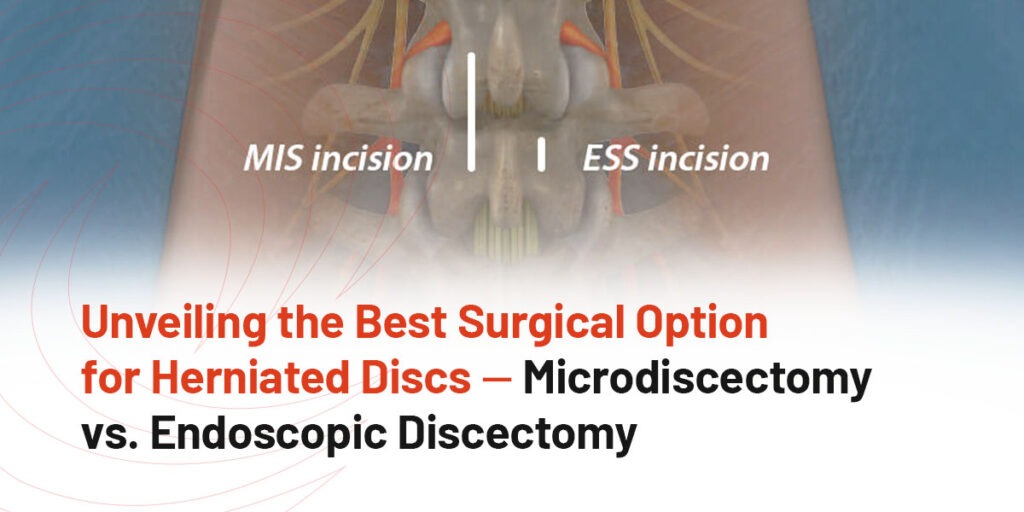
Fortunately, there are surgical options available to relieve the pain caused by herniated discs. Two common surgical approaches for this condition are microdiscectomy and endoscopic discectomy. In this blog post, we’ll compare these two procedures to help you decide which one might be right for you.
Living with the debilitating pain of a herniated disc can feel like an endless battle. Simple tasks become daunting challenges, and the prospect of returning to a pain-free life can seem like a distant dream. When deciding to have surgery for a herniated disc, you must weigh various factors to make the best choice for your well-being.
Microdiscectomy may provide the relief you seek if you’ve reached a point where conservative treatments do not succeed. This surgical procedure, often hailed as the gold standard for addressing herniated discs, offers the promise of relief and recovery. What is it, how does it work and what can you expect from this time-tested solution? Let’s look at how microdiscectomy can be the key to unlocking the shackles of herniated disc pain.
Endoscopic spine surgery is a game-changer that is redefining how spine surgeons operate. This cutting-edge, ultra-minimally invasive technique offers patients a path to recovery with smaller incisions, faster healing and less postoperative pain and discomfort.
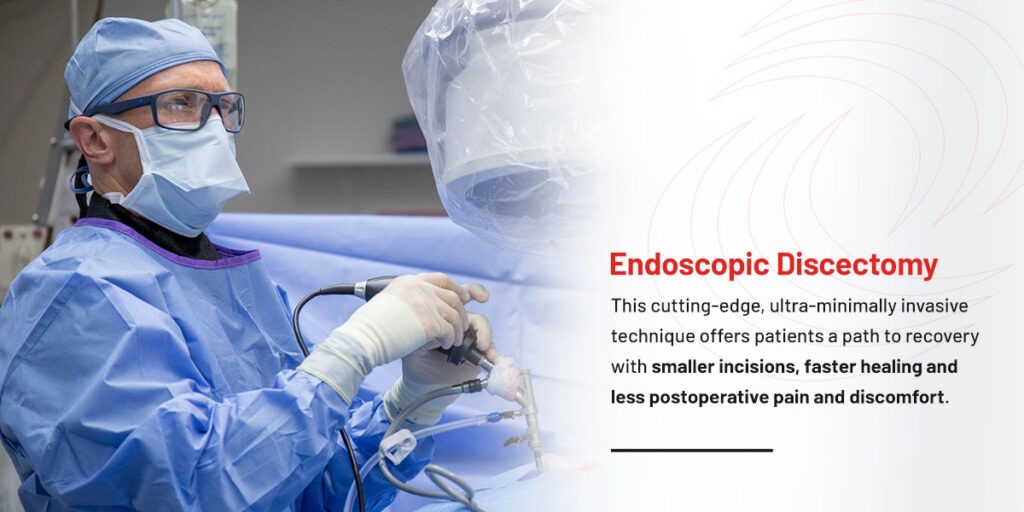
Endoscopic spine surgery offers numerous advantages over microdiscectomy surgery. Studies and clinical evidence have shown this innovative approach has many benefits, making it an attractive option for patients and surgeons.
One significant advantage of endoscopic spine surgery lies in its ability to expedite recovery. Many patients undergoing endoscopic procedures report reduced postoperative pain and discomfort, resulting in a swifter return to work and daily life, typically within two to four weeks. In contrast, conventional microdiscectomy surgeries may necessitate prolonged rehabilitation and downtime, affecting your overall quality of life and extending the minimum recovery period to six to eight weeks.
When considering which procedure works better for you, it is vital to also understand the risks you may face. Though both options are safe and most operations are successful, exploring the potential complications that could occur during each is still worthwhile to explore. However slim these chances might be, you should still know what they are before making your final choice.
Every surgical procedure brings a risk of complications, and the spine is a sensitive area and a vital body part. However, minimally invasive techniques are typically safer, with shorter recovery periods.
Several lifestyle-related factors might adversely affect surgical outcomes, procedure success and patient recovery. These include obesity, habits like smoking and jobs requiring heavy manual labor. Age is another variable that can affect the possibility of a complication occurring.
From minor problems that a surgeon can resolve in the moment to more serious issues that need further intervention, these are the procedure-related complications associated with microdiscectomies.
Compared to traditional surgical procedures, endoscopic discectomies cause fewer severe injuries or adverse outcomes. These complications could happen during and after an endoscopic discectomy.
Awake spine surgery offers distinct advantages, such as reduced reliance on general anesthesia, faster recovery times and real-time patient feedback during the procedure. Outpatient awake endoscopic spine surgery represents a significant advancement in minimally invasive spine procedures, offering a range of compelling benefits. By avoiding general anesthesia, patients experience fewer risks and side effects, making it a safer option for people with specific health concerns. The outpatient setting allows for a quicker return home, reducing hospital costs and minimizing the risk of hospital-acquired infections.
Endoscopic spine surgery represents a significant step forward. The studied benefits are clear and compelling, including faster recovery, the potential for outpatient treatment, less damage to surrounding tissues and enhanced precision. As technology continues advancing, endoscopic spine surgery will become an even more attractive option for patients seeking relief from spinal conditions. However, you should only choose surgery after consulting with a qualified medical professional who will evaluate your specific condition and needs.
Choosing between microdiscectomy and endoscopic discectomy can be a pivotal decision for spine patients seeking relief from the discomfort of herniated discs. The decision hinges on several crucial factors. Microdiscectomy has a well-established track record and is the most commonly used procedure by spine surgeons. On the other hand, endoscopic discectomy stands out as an ultra-minimally invasive alternative, ideal if you want a swifter recovery.
Your surgeon’s expertise is paramount in this choice. Engaging in open communication with your health provider, sharing your preferences and considering each option’s pros and cons will ultimately guide you toward the procedure best suited to your needs.
Whether it’s the reliability of microdiscectomy or the appeal of minimally invasive endoscopic discectomy, both paths lead to the common goal of alleviating your pain and restoring your quality of life. Contact us at DISC to make an appointment or request a second opinion.