The anesthesiologist will administer an anesthetic. Once sedated, the operating room staff will position you comfortably on your stomach on the operating room table. Your back will be cleansed, sterilized, and prepped for the procedure to start.
Kyphoplasty and vertebroplasty are effective treatment options to reduce pain caused by a vertebral body compression fracture.
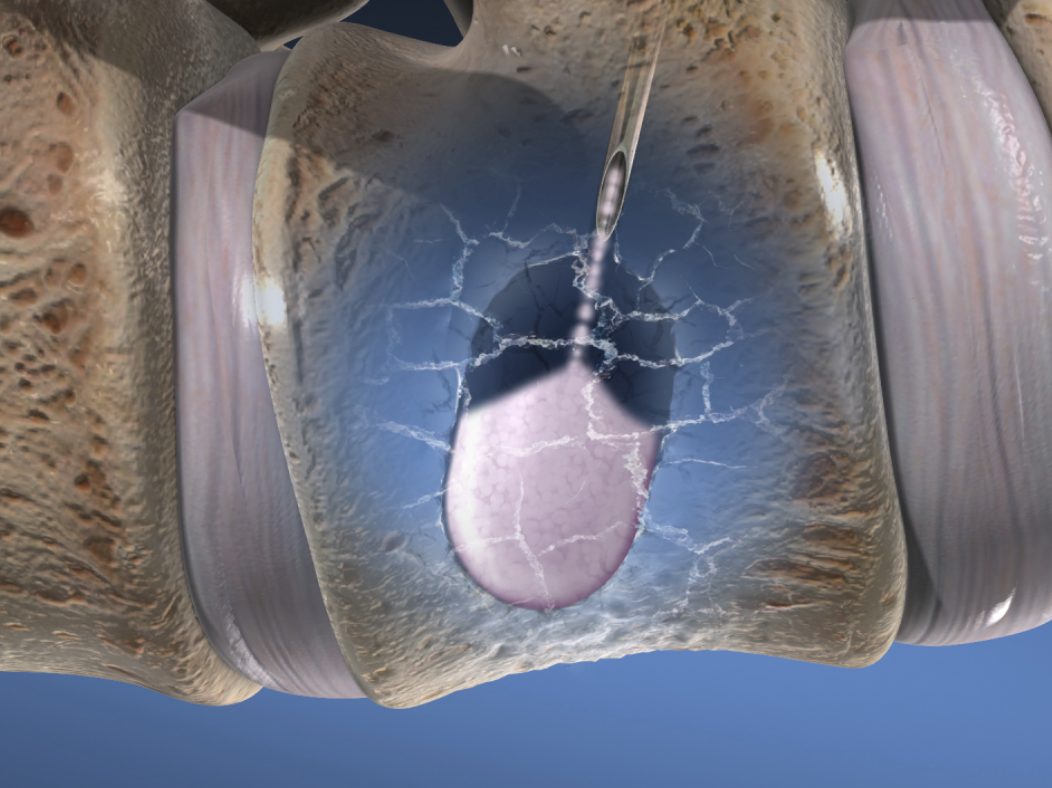
Vertebroplasty works percutaneously through the skin to inject bone cement into the vertebral body’s cancellous bone to stabilize the fracture and alleviate pain. The cement interdigitates within the fracture crevices.
Kyphoplasty utilizes an inflatable balloon deployed in the fractured vertebral body creating a cavity for the cement to be injected. The balloon potentially restores the height of the vertebral body and improves alignment by reducing kyphosis (outward curvature of the spine, causing hunching of the back).
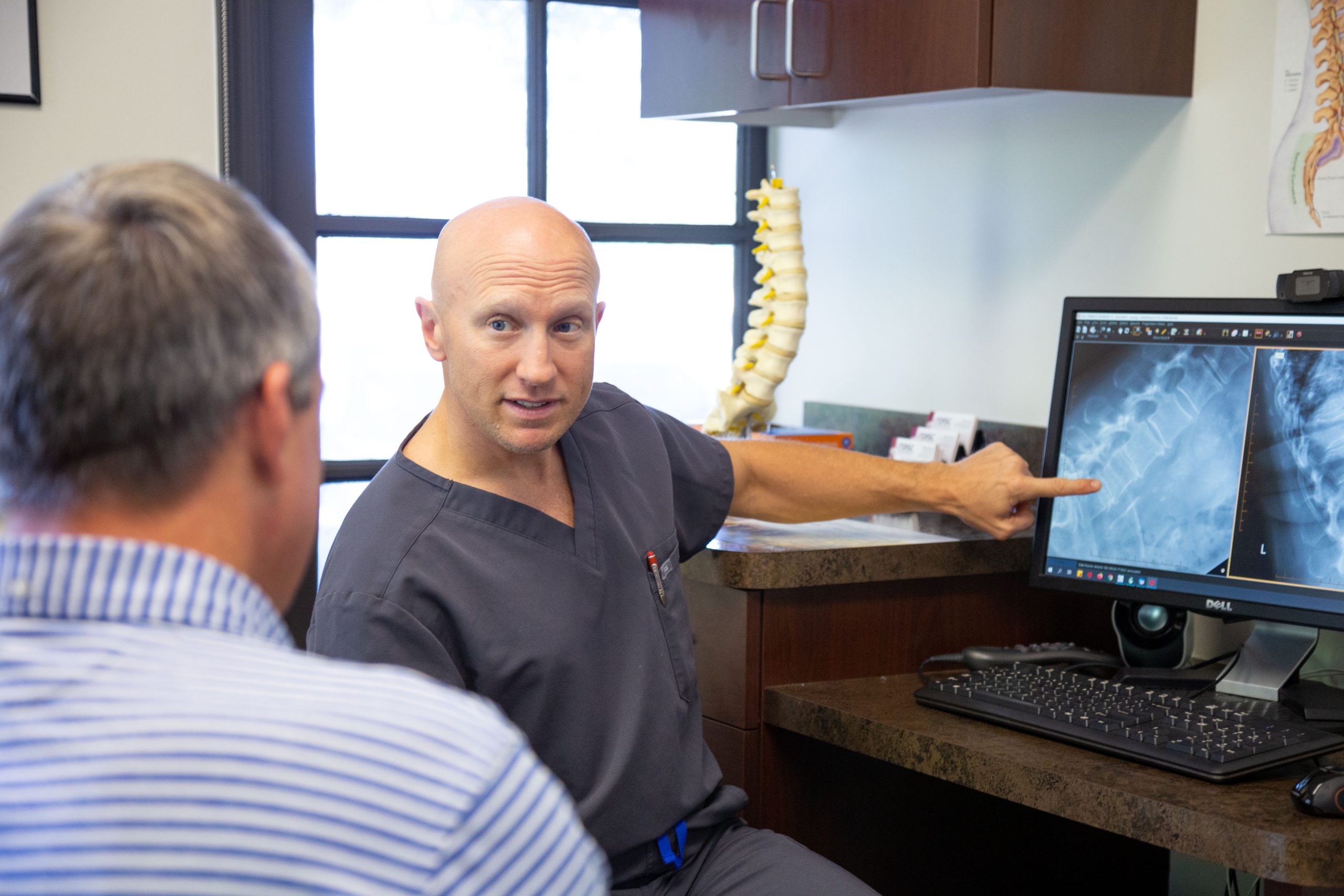
Patients with increasingly painful back pain caused by osteoporosis or vertebral compression fractures may be good candidates for vertebroplasty or kyphoplasty.
Patient candidates for these procedures typically have reduced physical function and ability to move because of the fractures in their spine.
Vertebroplasty is a medical procedure used to treat compression fractures in the spine, particularly those caused by osteoporosis or cancer. The procedure involves injecting a special cement-like material into the fractured vertebra to stabilize it and alleviate pain. The ideal candidate for vertebroplasty typically meets the following criteria:
The anesthesiologist will administer an anesthetic. Once sedated, the operating room staff will position you comfortably on your stomach on the operating room table. Your back will be cleansed, sterilized, and prepped for the procedure to start.
Your surgeon will begin by injecting a local numbing anesthetic in the area over the fracture vertebrae is located. Under fluoroscopic guidance, the surgeon directs a hollow needle called a trocar through your skin to the affected center of the fractured vertebra.
Through the trocar needle, the surgeon deploys a balloon in the collapsed vertebra. The balloon is then inflated, which creates a cavity and may distract the vertebral endplates to restore vertebral height. The balloon is then deflated and removed.
Both vertebroplasty and kyphoplasty inject bone cement which fills and stabilizes the fracture. The amount of cement and pressure is constantly monitored under fluoroscopy to avoid leaks into the spinal canal. Stabilizing the fracture will significantly reduce the pain.
The needle/trocar is removed, the small incision is dressed with Steri-Strips placed on the skin and an additional bandage is applied. Once the bone cement has hardened, the patient is moved from the operating room table to the stretcher and taken to recovery for a short period.


Try to walk 5-10 minutes every few hours and gradually increase the walking duration as you feel able to. After the first 72 hours, you can increase physical activities as tolerated and return to all physical work.
The following symptoms can indicate a potential problem. You should call the office to notify the surgeon as soon as possible.
If you have any questions after surgery or experience these symptoms, please call 602-944-2900. Our on-call service will answer calls after hours, and they will page the surgeon in case of an emergency. Otherwise, calls will be returned the following business day.

The kyphoplasty procedure has been performed on more than 1 million patients safely and effectively over the past 20 years. Balloon kyphoplasty has been clinically proven to relieve pain and restore vertebral body height and deformity. Patient benefits from kyphoplasty include:
The safety of kyphoplasty/vertebroplasty is like nonsurgical measures with a low complication rate. As with any surgical procedure, there are potential for serious adverse events; however, low such as:
Other risks can include – infection and leakage of bone cement into surrounding tissue around the spinal cord. On rare occasions, there can be a risk of paralysis and cement leaking into blood vessels resulting in damage to vessels, lungs, and heart.
You have two options if you have been diagnosed with an acute spinal vertebral compression fracture. You may be prescribed pain medication and bed rest until it heals over several weeks or months (nonsurgical measures). The other option is a surgical procedure called kyphoplasty or vertebroplasty which can stabilize the fracture. Your physician can refer you to a specialist who performs kyphoplasty. They can explain the benefits, risks, and if you are a good candidate for the procedure.
As previously explained above, both procedures are similar in that they are ultra-minimally invasive surgical procedures that treat vertebral compression fractures of the spine. Both procedures are vertebral augmentation that relieves back pain and stabilizes a spinal fracture using bone cement. Kyphoplasty, unlike vertebroplasty, utilizes a balloon to expand the fracture and injects cement. This procedure has been shown to restore vertebral body height.
Both vertebral augmentation procedures take about a half hour per spinal level treated. The procedures are ultra-minimally invasive, and if performed outpatient at a surgery center or office procedure room, patients go home the same day. If performed at a hospital, patients generally go home the next day.
Most patients experience pain relief and improved mobility within 48 hours and, in some cases, immediately after surgery. Most patients can return to work a day or two later once the pain from the incisions has subsided. There are usually no physical restrictions after 72 hours, and the patient’s pain has been relieved.
Your physician can explain the benefits, risks, and if you are a good candidate for the Kyphoplasty/Vertebroplasty procedure.
Our spine health blog features up-to-date spine education and expert spine tips from our spine specialists here at DISC.
1635 East Myrtle Avenue Suite 100, Phoenix, AZ 85020, USA
18700 North 64th Drive Suite 105, Glendale, AZ 85308, USA
8630 East Vía de Ventura Suite 210, Scottsdale, AZ 85258, USA
3487 South Mercy Road, Gilbert, AZ 85297, USA
1635 East Myrtle Avenue Suite 400, Phoenix, AZ 85020, USA