What Is Anterior Cervical Decompression and Fusion Surgery?
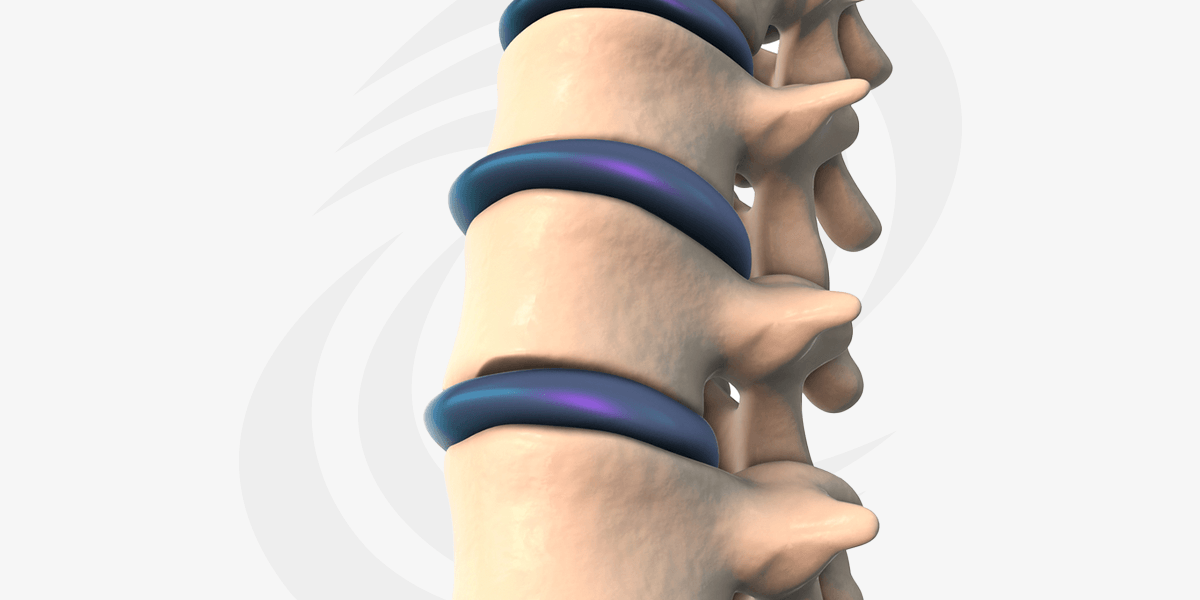
An anterior cervical discectomy and fusion (ACDF) is a surgical procedure performed to treat certain conditions affecting the neck and cervical spine. The goal of the procedure is to relieve pressure on the spinal cord or nerve roots and stabilize the affected area of the spine.
During an ACDF, the surgeon makes an incision in the front of the neck to access the cervical spine. The muscles and tissues are gently moved aside to expose the problem disc or discs. A discectomy is then performed, which involves removing the damaged or herniated disc(s) that may be compressing the spinal cord or nerve roots.
After the disc is removed, the space between the adjacent vertebrae is usually filled with a bone graft. The bone graft promotes fusion, which is the process of joining the two vertebrae together to form a single, solid bone. The graft may be taken from the patient’s own body (autograft) or obtained from a bone bank (allograft). The surgeon then places a titanium metal implant called a cervical plate with screws to provide additional stability during the fusion process.
The fusion process typically takes several months to complete. During this time, the bone graft gradually fuses the vertebrae together, resulting in a solid bone bridge. This fusion helps to stabilize the spine, relieve symptoms, and prevent further degeneration or movement between the vertebrae.