Endoscopic spine surgery (ESS) is an ultra minimally invasive surgical procedure that effectively relieves chronic low back and leg pain.
This state-of-the-art spine surgery utilizes an HD camera attached to an endoscope inserted through a ¼ inch skin incision to the target pain generator in your spine.
The endoscopic orthopedic procedure allows spine surgeons to operate safely, with greater accuracy, and offer patients better outcomes.
The surgeon can observe the spine on an HD monitor and operate through the endoscope using highly specialized micro-instruments like a laser, radiofrequency probe, or graspers.
An HD endoscope with an attached HD camera is inserted into the cannula or often called a tubular retractor. The surgeon can now visualize on an HD monitor the spinal canal, vertebral disc and exiting nerves. Endoscopic spine surgery can treat effectively herniated disc, bulging disc and foraminal stenosis.
This ultra minimally invasive spine surgery is the most effective surgical technique that relieves a herniated disc, low back pain, and sciatica. Because it utilizes a 1/4 inch incision, patients recover faster than minimally invasive spine surgery.
This endoscopic spine surgery effectively treats painful conditions caused by a herniated disc, spinal stenosis, sciatica, and facet joint syndrome. This procedure is an excellent solution for patients suffering from pain seeking a faster return to an active lifestyle.
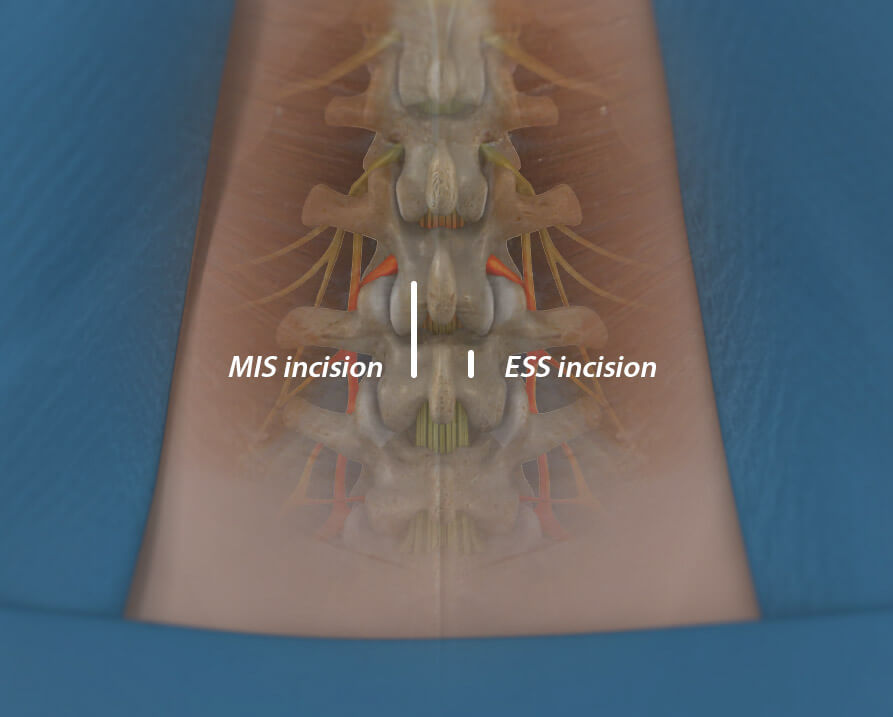
Minimally invasive spine surgery (MIS), the standard of care in spine surgery, represents a broad spectrum of techniques, with endoscopic being the least invasive. Endoscopic spine surgery is as effective as the MIS microdiscectomy procedure at relieving painful spine conditions.
However, unlike MIS, endoscopic spine surgery significantly reduces trauma to the patient’s muscles and soft tissue leading to faster recovery. The endoscopic procedure utilizes a surgical approach that avoids the major stabilizing muscles of the lower back.
Unlike the MIS incision of one inch or more, ESS uses a ¼ inch incision. Smaller surgical incisions and avoiding major back muscles can significantly improve patient outcomes.
Sometimes called ultra-minimally invasive, the endoscopic spine surgery technique can be performed faster, allowing the surgeon better access to the spinal nerves and disc, and superior visualization. Also, ESS requires no general anesthesia, which affords patients less risk and faster discharge from the hospital within 2-3 hours of surgery.
Image for illustrative purposes only. Your physician will determine the actual incision placement.
This is the most common least invasive procedure used to relieve the pressure of a herniated disc on a spinal nerve causing pain. It is also called Selective Endoscopic Discectomy, utilizing the world’s first working channel endoscope to perform direct visualized endoscopic spine surgery.
Endoscopic Facet Medial Branch Nerve Transection is an ultra-minimally invasive endoscopic procedure treating chronic low back pain caused by facet joints in your back. This procedure has been shown to provide up to five years of long-term relief. If you had short-term relief from a pain management radiofrequency ablation procedure, you might be a candidate.
This is an ultra-minimally invasive endoscopic laser spine surgery that targets foraminal stenosis, also called lateral recess stenosis. Lateral recess stenosis can be the cause of failed back surgery in up to thirty percent of patients. The endoscopic technique utilizes motorized burrs and a side-firing laser to enlarge the narrow boney foramen, thus relieving the exiting spinal nerve’s pressure. Endoscopic Foraminoplasty may help select patients avoid a minimally invasive spinal fusion.
Endoscopic spine surgery is the least invasive surgical option for patients suffering from back and leg pain. Endoscopic spine surgery treats multiple painful spinal conditions such as:
The ideal candidate for endoscopic spine surgery can vary depending on the specific condition being treated and the surgeon’s assessment. However, in general, the following characteristics may make a patient a good candidate for endoscopic spine surgery:
Our candidate selection process begins with our proprietary Personalized Pain Mapping. Personalized pain mapping of the spine, also known as diagnostic spinal mapping, is a procedure performed to identify and locate the source of a patient’s chronic or persistent spinal pain. It is a diagnostic tool used by spine specialists to gain a better understanding of the specific areas causing pain in an individual patient.
We listen carefully to your pain journey and your desired outcomes. Then we use diagnostic and therapeutic injections to pinpoint the pain generator. We personalize a treatment plan that will effectively address your pain and desired outcomes. Many of our patients get better without any surgical intervention. However, those patients we select for endoscopic spine surgery have great results and a high level of satisfaction.
Personalize pain mapping of the spine allows for a more accurate diagnosis and helps our expert spine specialist tailor the least invasive and most effective treatment options for patients.
If you are seeking a second opinion or looking to travel for a less invasive surgery, our orthopedic spine specialists in Phoenix are available to help you get an accurate spine diagnosis and customize an innovative treatment plan to get back to enjoying life. Schedule an appointment with one of our compassionate expert spine surgeons today.
Our spine health blog features up-to-date spine education and expert spine tips from our spine specialists here at DISC.
1635 East Myrtle Avenue Suite 100, Phoenix, AZ 85020, USA
18700 North 64th Drive Suite 105, Glendale, AZ 85308, USA
8630 East Vía de Ventura Suite 210, Scottsdale, AZ 85258, USA
3487 South Mercy Road, Gilbert, AZ 85297, USA
1635 East Myrtle Avenue Suite 400, Phoenix, AZ 85020, USA