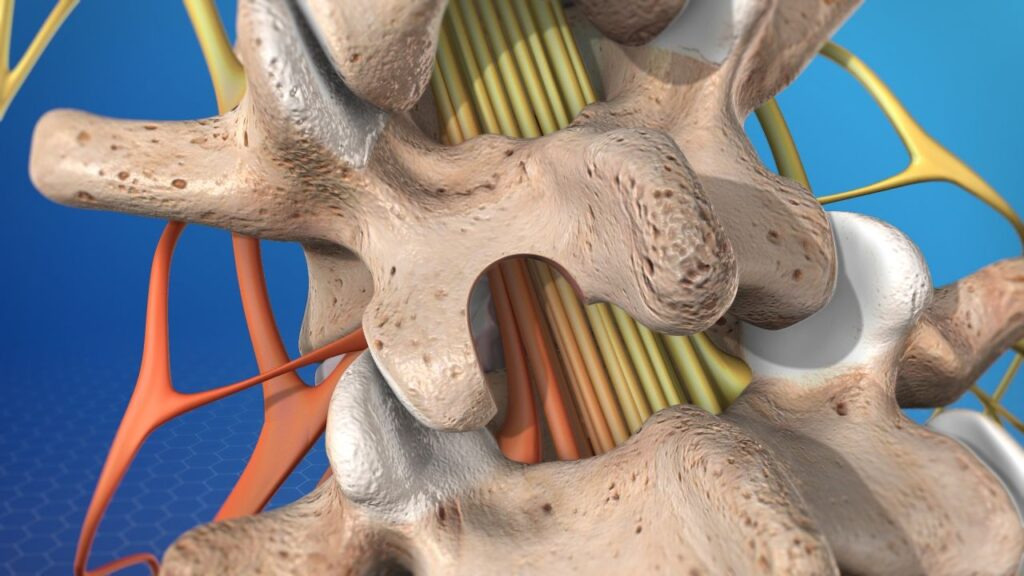
Spinal stenosis is compression or narrowing that can result in pressure or pinching on the nerve structures and cause one or both legs to be in pain. The typical sciatica pain is an example of pinching of nerves in the lower lumbar spine and may be caused by one of the following:
A surgery that is often recommended for these problems is a lumbar laminectomy. As spine surgeons, we perform the laminectomy procedure with almost every lumbar surgery that we complete. The traditional technique was first described in the early 1900s. The muscles attached to the posterior aspect of the spine are dissected off the spine on either side of the spinal column. These muscles attach to the lamina and spinous processes which act as levers in a pully system. To gain access to the nerves contained within the spinal canal, the lamina and spinous processes are removed. Any structures that are compressing the nerves are removed as well to free the nerve structures from compression. This may include bone and soft tissues such as herniated disc material.
Laminectomy is an effective procedure for relieving pressure on spinal nerves, but during the procedure, the removal of some of the structures creates collateral damage. The muscle attachments to the spinous processes have an important biomechanical function. The resulting weakness and limited motion can have deleterious effects on the spine. Furthermore, the removal of connecting tissues such as ligaments between bones can create destabilizing effects.
In some patients, excessive spinal destabilization and muscle damage from laminectomy may result in:
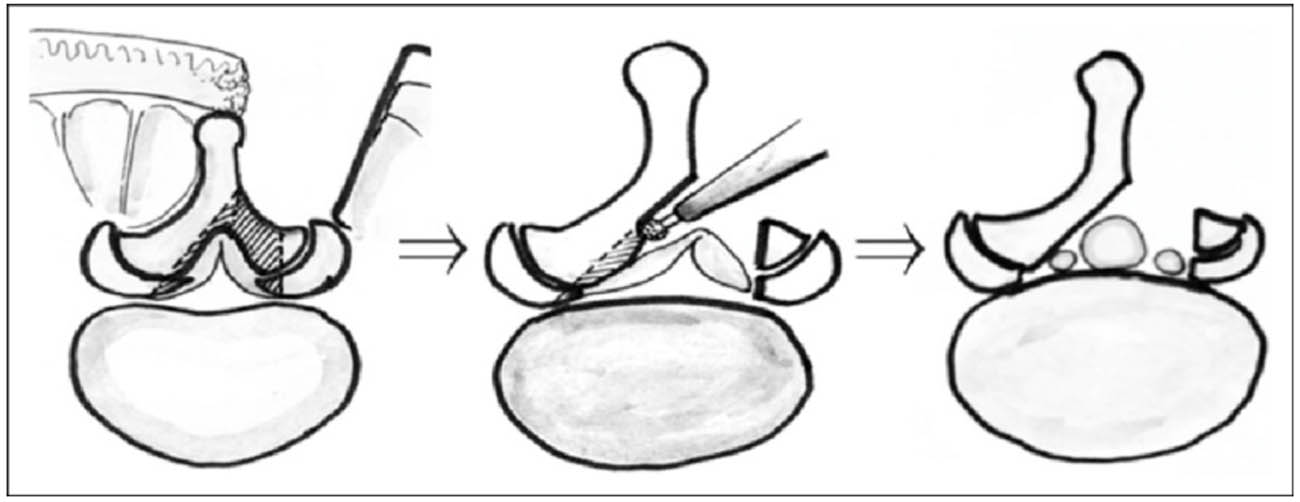
During the 1980s, and with the introduction of the operating microscope, Dr. John McCulloch described a less invasive technique for decompressing spinal nerves. The McCulloch laminectomy (also known as lumbar laminoplasty or unilateral laminectomy with bilateral decompression) spares many of the supporting structures previously described.
In contrast to traditional laminectomy, the spinal musculature is dissected away from the spinal bones only on one side. During the procedure, the lamina, spinous process, inter-supraspinous ligaments are preserved. Enough of the lamina is removed under the microscope to gain access to the spinal canal and nerve structures. Then with a slight rotation of the bed and repositioning of the microscope, the lamina is undermined to the contralateral side. The nerves contained in the spinal sac are directed aside enough to gain access across the canal space and removes tissues that are compressive of the nerves. This is depicted in the image below in some detail (credit ResearchGate.net).
If you have been recommended to have surgery on your lower back, make an appointment to be seen for a second opinion to see whether you would be a candidate for this minimally invasive laminectomy technique.
In the pictures, you see before and after images of the same patient’s lumbar MRI. The patient had degenerative disc disease that caused areas of severe spinal canal stenosis and spondylolistheses at lumbar 3 on 4 and lumbar 4 on 5. The patient had been recommended a 3-level lumbar fusion surgery. Because of severe health issues and a history of osteoporosis, major surgery such as the one recommended was not possible. Instead, we opted for unilateral lumbar laminotomies with bilateral decompression. This allowed significant relief of pressure on the nerve structures in the spinal canal and demonstrated in the second picture. The midline bone structures known as the spinous processes along with their muscle attachments were fully preserved on the right side as the approach was made from the left side only.
MRI Pre-Surgery Showing Spinal Cord Compressed
MRI Showing Decompressed Spinal Cord After Surgery