April 4, 2025
What Is a Pinched Nerve?
A pinched nerve, also known as radiculopathy in medical terms, is a condition in which one or more nerves are compressed or “pinched” and unable to function properly. This happens when the nerve suffers from too much pressure caused by surrounding tissues, such as bones, muscles, cartilage and tendons. Nerves function like electrical cables, transmitting signals between the brain, spinal cord and the rest […]
March 15, 2025
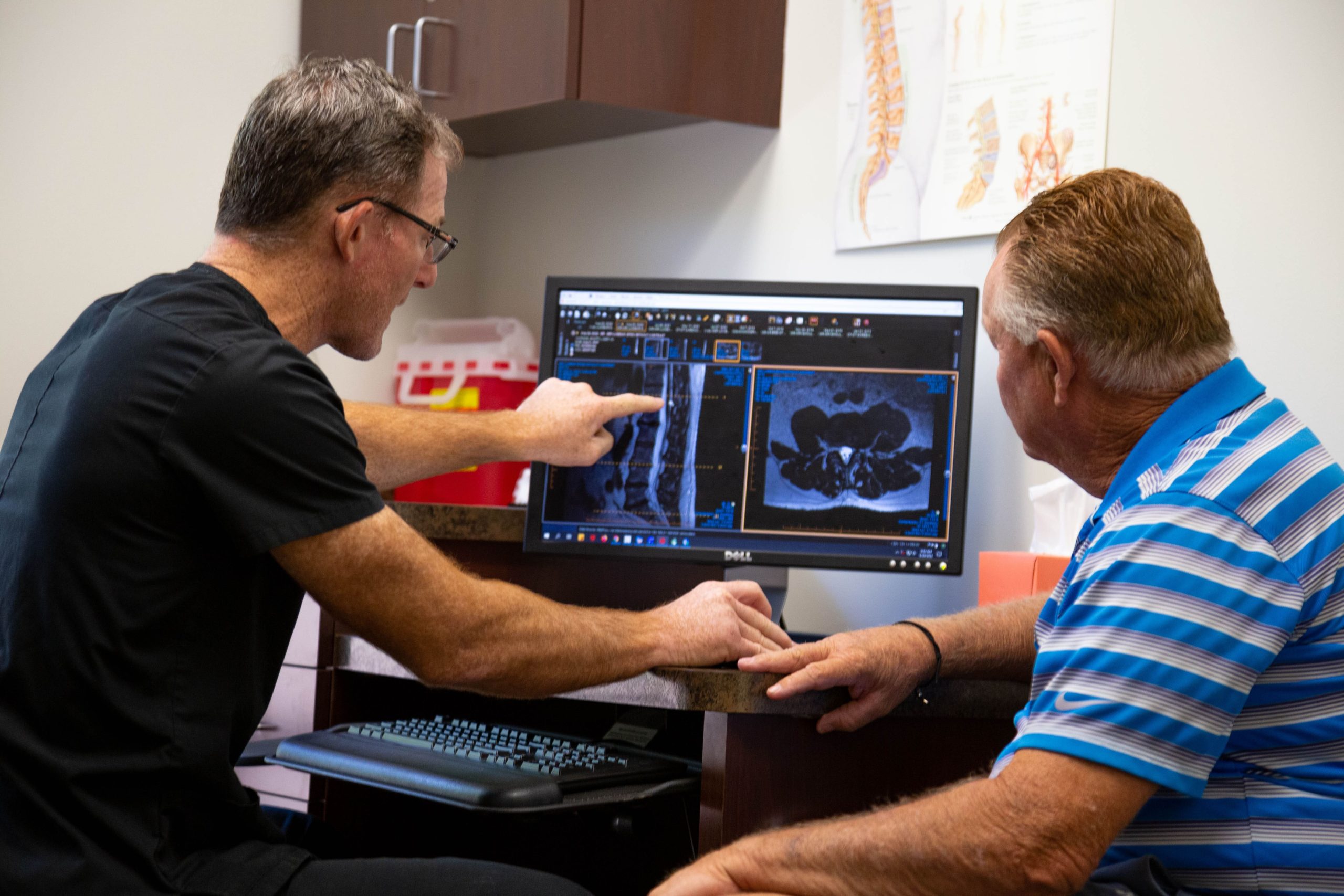
Spine Surgery Consultation Questions
Any surgery can be intimidating, especially if you haven’t undergone one before. It’s natural to have questions about the process, including before-and-after care, to ensure a smooth process. Asking questions about your surgery can help prepare you for the event and provide peace of mind. Below are questions you may want to ask your surgeon […]
February 10, 2025
Everything You Need to Know About Sciatica: The Essential Guide
Are you tired of dealing with nagging back pain that radiates down your leg? You may be experiencing sciatica — a common but complex condition affecting the sciatic nerve, often leading to sharp, shooting pain from the lower back down to the legs.

January 2, 2025
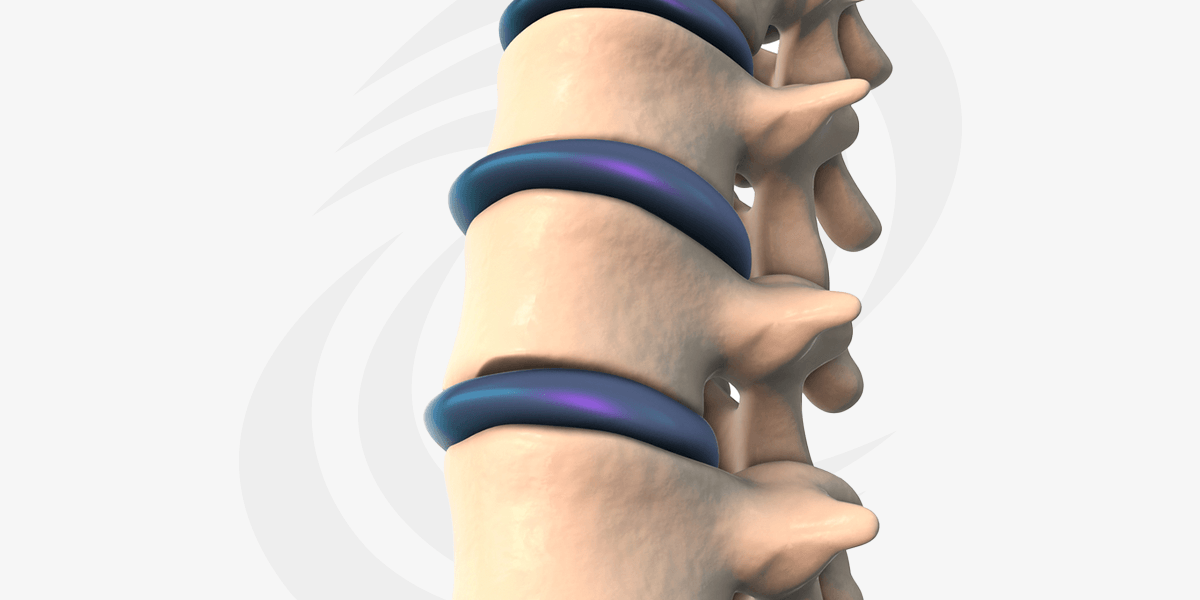
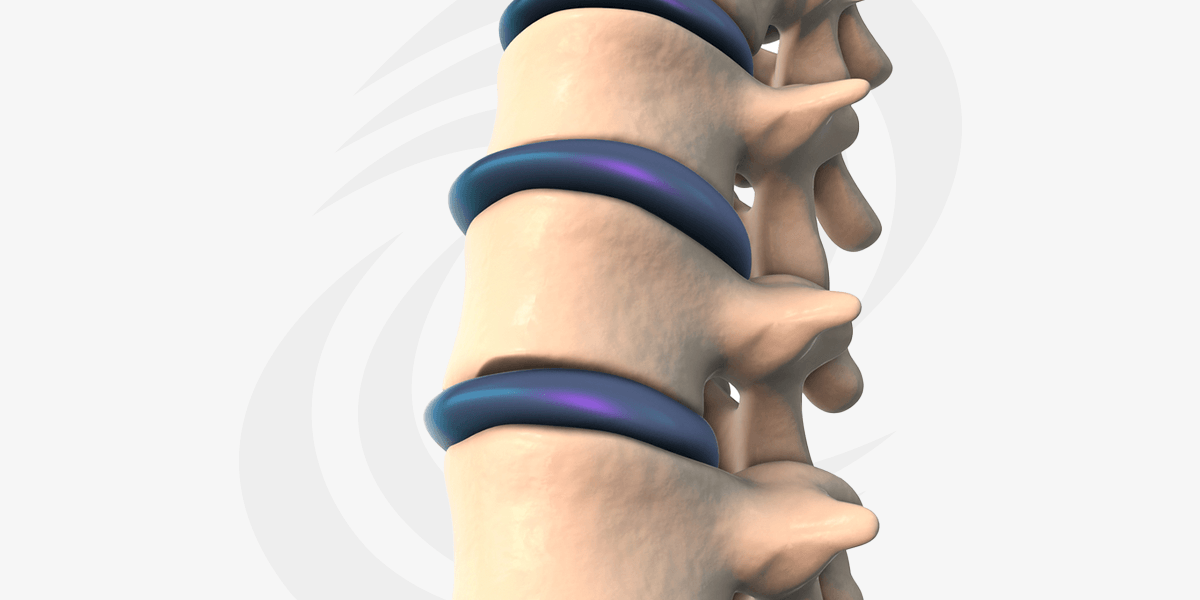
Pros and Cons of Cervical Artificial Disc Replacement
If you’re reading this, chances are you’ve been living with chronic neck pain, perhaps caused by conditions like degenerative disc disease, herniated discs or cervical radiculopathy. The discomfort can range from mild annoyance to debilitating pain, affecting everything from your ability to work to your quality of life. But you’re here because you’ve […]

December 26, 2024
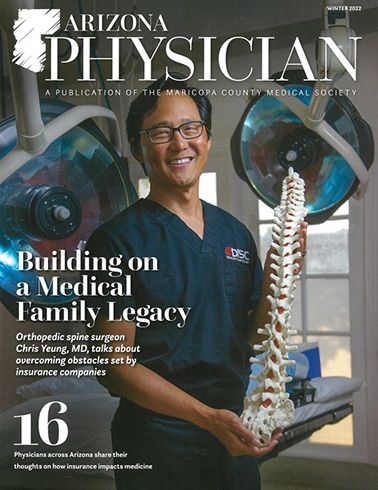
Why Canadians Suffering From Spine Pain Should Choose DISC
December 23, 2024
Cervical Artificial Disc Replacement Recovery Time
Are you considering or have recently undergone a cervical artificial disc replacement? If so, you’re on the path to relief. Chronic neck pain caused by degenerative disc disease or herniated discs can be debilitating. This advanced procedure removes and replaces a damaged disc with a prosthetic one. It preserves and restores neck motion. The result […]
November 25, 2024
What Is The Cost of Cervical Total Disc Replacement?

November 20, 2024
Understanding Recovery After Spinal Surgery: What to Expect and How to Heal