How Soon Can One Expect to Feel Better After Treatment?
Recovery after spinal decompression surgery, such as a lumbar laminectomy or discectomy, typically takes around 4-6 weeks, though this timeline varies based on individual factors like age, overall health and the underlying cause of nerve compression.
During this period, patients gradually increase their activity levels as the surgical incision heals and stitches are removed. Those with sedentary jobs that require minimal physical exertion may return to work within about four weeks, while individuals with physically demanding roles may require up to four months of recovery before resuming their duties.
Surgical healing is only one component of recovery from cauda equina syndrome. The damaged nerves must also repair themselves, a process that often extends well beyond the healing of the incision. Nerve recovery can take months and, in some cases, years.
Patients experiencing lingering issues such as leg weakness, instability, or difficulties with bowel and bladder control may benefit from physical or occupational therapy. Assistive devices like walkers or canes and bladder retraining programs can be critical in facilitating daily activities and improving quality of life during this recovery period.
Additional strategies may be necessary for patients with severe and persistent nerve damage. These can include self-catheterization and bowel management techniques while awaiting nerve regeneration, which may take 18 months to two years or longer. In certain cases, the damage may be permanent, requiring patients to adopt adaptive devices or support systems to maintain their independence.
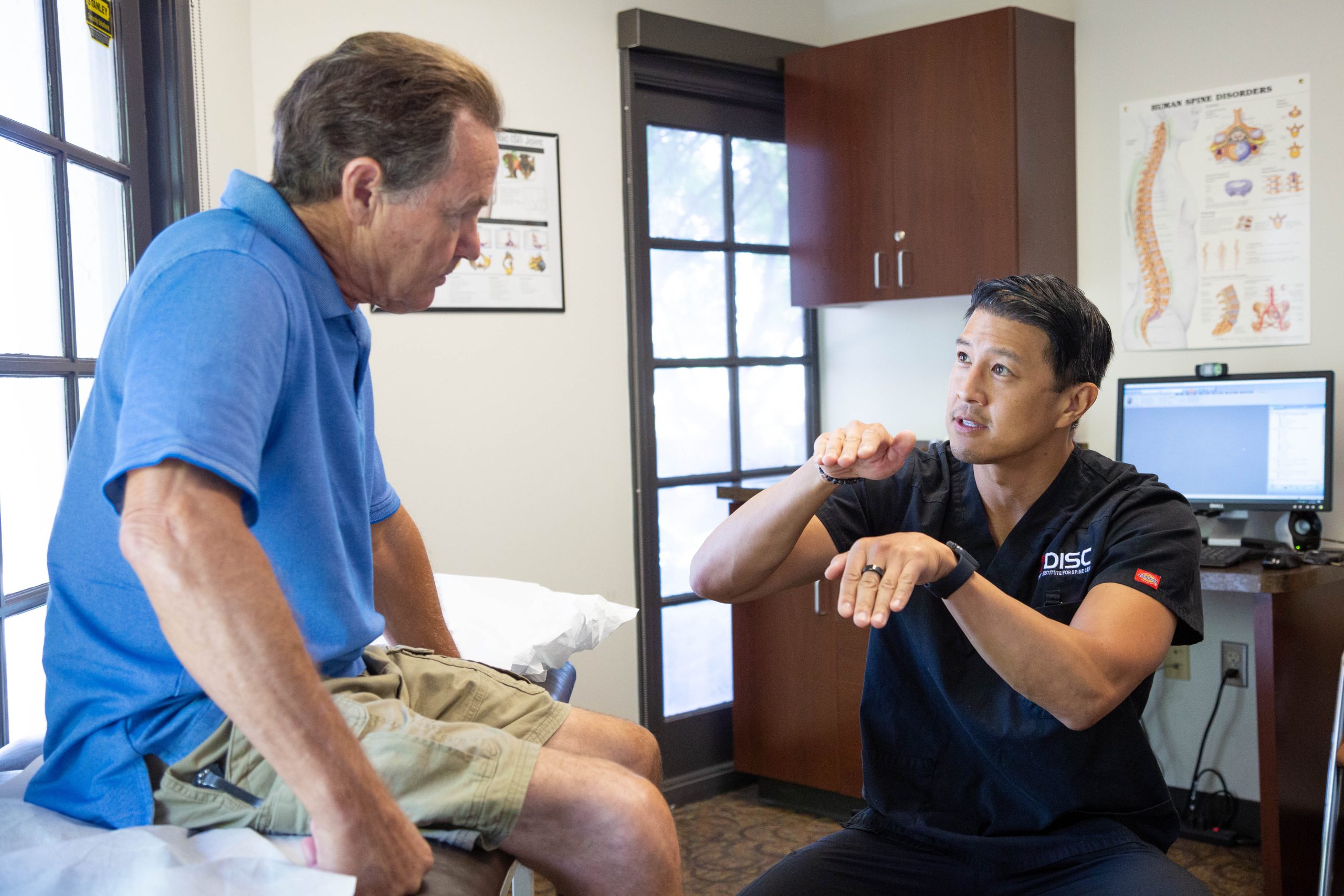
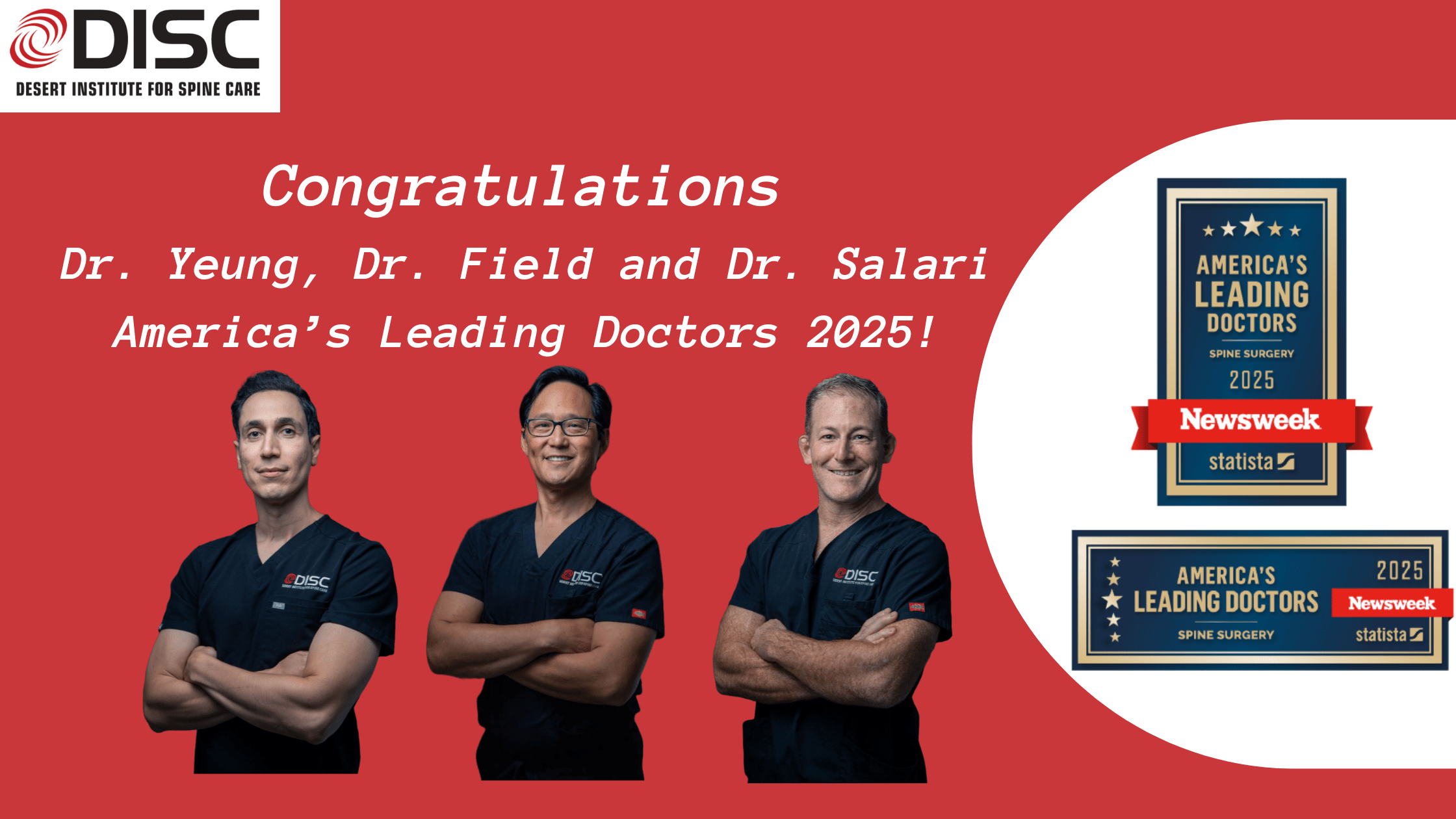
Despite these challenges, with prompt and comprehensive treatment, many individuals with cauda equina syndrome regain significant function in their legs and lower body. By working closely with experienced specialists, patients can receive personalized care plans tailored to their unique needs, enabling them to achieve the best possible recovery outcomes.