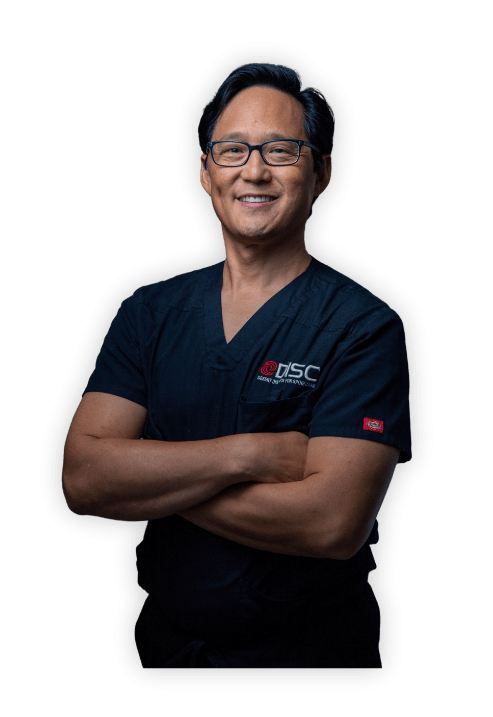
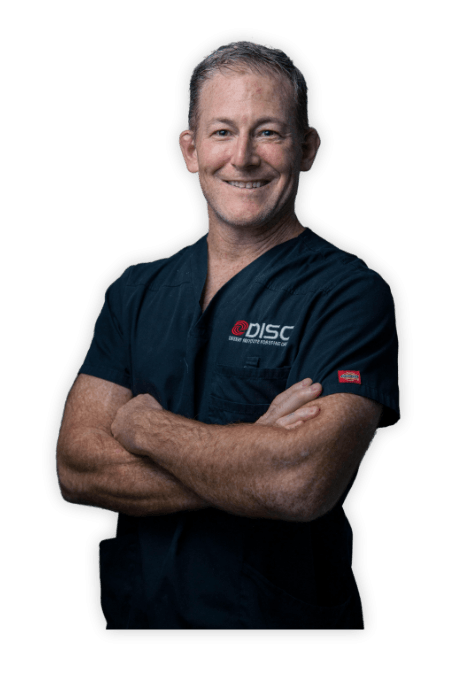
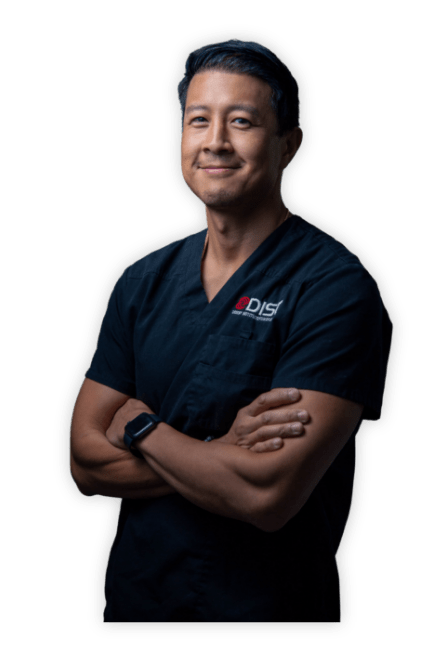
Meet the Doctor
Christopher A. Yeung, M.D.
- Top Doc Award by Phoenix Magazine for 2009 – 2010, 2012 – 2025
- Phoenix Magazine’s TOP DOCTOR – 10 years Excellence Award














3487 South Mercy Road, Gilbert, AZ 85297, USA
1635 East Myrtle Avenue Suite 400, Phoenix, AZ 85020, USA
8630 East Vía de Ventura Suite 210, Scottsdale, AZ 85258, USA
1635 East Myrtle Avenue Suite 100, Phoenix, AZ 85020, USA
18700 North 64th Drive Suite 105, Glendale, AZ 85308, USA