A procedure that treats and removes herniated discs and spinal stenosis within the low back.
Ultra-minimally invasive spine surgery is a form of minimally invasive surgery that can reduce scarring and promote better patient outcomes. The experts at the Desert Institute for Spine Care (DISC) are here to help you find the right solution for your spine condition.
Ultra-minimally invasive spine surgery (Ultra-MISS) is a group of advanced surgical procedures that significantly improve patient satisfaction and quality of life after spine surgery. These least invasive procedures represent the most technologically advanced improvements in spine surgery techniques in the past 20 years.
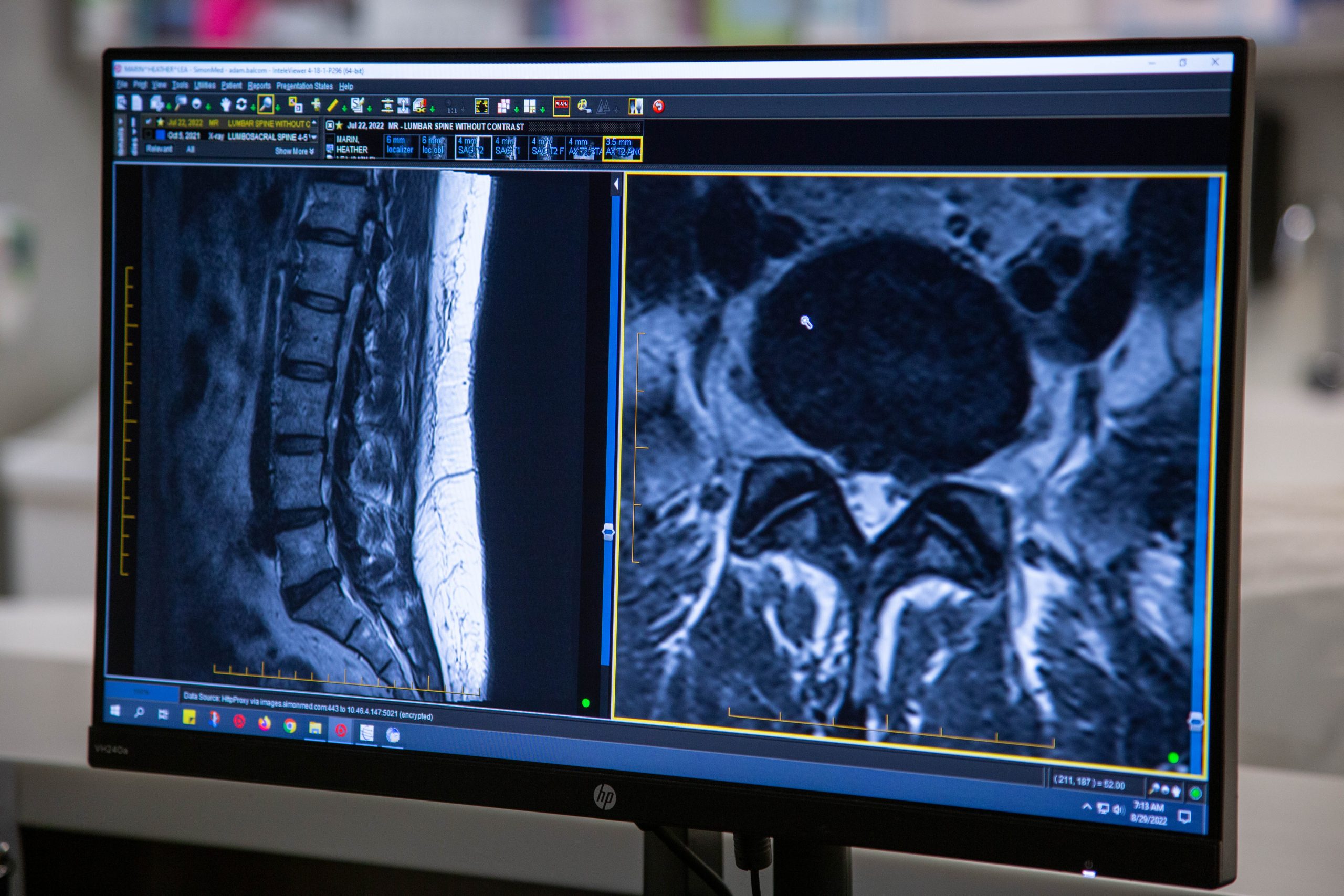
The Ultra-MISS procedures are performed through a micro-incision of ¼ inch utilizing fluoroscopic (X-ray) guidance and an HD endoscope/camera. The key patient benefits of Ultra-MISS are less post-operative pain and faster recovery times, allowing patients to return to work and physical activity sooner than with minimally invasive spine surgery (MISS).

The overall goal of ultra-minimally invasive spine surgery is to utilize the least invasive procedure to alleviate pain before considering more invasive surgery.
Two significant developments in spine surgery over the past 30 years have been the transition from traditional open spine surgery to minimally invasive surgery and the advent of ultra-minimally invasive surgery.
The goal of traditional spine surgery and minimally invasive spine surgery is the same — decompress spinal nerves and stabilize abnormal spine movement. Traditional surgery or open surgery is effective. However, because of the large incisions, there were many complications, and patients endured significant post-operative pain and recovery times.
Minimally invasive surgery (MIS) was developed to achieve similar outcomes to traditional spine surgery, minimizing muscle dissection, collateral damage to soft tissue and disruption of ligament attachment sites. MIS significantly reduced the patient’s blood loss, complication rates and recovery times.
Minimally invasive spine surgery allows surgeons to use metal tubular retractors with 1- to 2-inch incisions instead of 3- to 5-inch large open incisions with traditional open surgery.
The MISS tubular retractor system gently dilates muscles rather than dissecting or cutting muscle. This significantly reduced the size of the incision, impact on patients’ muscles and postoperative pain.
However, there was still room for improvement in the surgical approaches through a smaller tubular retractor to reduce muscle and ligament trauma, resulting in less post-operative pain and faster recovery time and return to work.

Over the past three decades, spine surgery has made significant advancements in surgical techniques, technology and instrumentation. Endoscopic spine surgery (ESS) is the foremost example of this advancement. Endoscopic spine surgery is a collective group of surgical approaches with highly specialized instrumentation that accomplishes the same decompressive goals of traditional and minimally invasive spine surgery.
Endoscopic spine surgery was the first ultra-minimally invasive spine (Ultra-MISS) procedure developed by the founder of the Desert Institute for Spine Care, Dr. Anthony Yeung. A pioneer, Dr. Yeung developed the Yeung Endoscopic Spine Surgery (YESS) technique and instrumentation, which utilizes an HD endoscope and 1/4-inch cannula access system to target and treat pain generators in the spine. The combination of Dr. Yeung’s new surgical approaches and advanced endoscopic high-definition imaging devices, coupled with specialized micro-instruments, has revolutionized spine surgery and patient satisfaction.
Many patients prefer Ultra-MISS because of the following advantages:


Ultra-MISS is an evolving philosophy of utilizing the least invasive yet most effective procedure to treat patients with painful spine conditions before ever considering minimally invasive surgery. Typically, patients suffering from spinal conditions will see pain management doctors after failing conservative treatment and pain medications prescribed by their primary care physician. Pain management physicians utilize diagnostic injections to pinpoint a painful spinal area. These injections can be therapeutic for a short period of time. Some patients who respond favorably to injections will be recommended for pain procedures like a radiofrequency facet ablation or RFA. This procedure targets the medial branch nerve which causes low back pain related to facet disease.
Radiofrequency ablation procedure provides low back pain relief. After about six months, the pain comes back, and the RFA can be repeated, or the patient is referred to a spine surgeon for consultation for chronic spine pain. The short-term results are due to the procedure being performed under fluoroscopic X-ray and not visualized by the doctor’s eye. RFA under X-ray puts a lesion on the nerve instead of severing it, and in 6 months, the nerve regenerates and is painful once again.
Dr. Anthony Yeung saw this short-term relief with pain management as an opportunity to develop an endoscopic facet rhizotomy procedure that visualized the painful nerve with an HD endoscope. Thus, when the surgeon identifies the painful nerve, they can ablate, sever and disconnect the pain signal. The endoscopic rhizotomy results in long-term low back pain relief lasting up to 5 years. Endoscopic spine surgery patients have better satisfaction and long-term relief and are able to return to an active lifestyle sooner.
Spine surgeons who take the time to train in this orthopedic subspecialty can provide patients with two significant benefits:
Ultra-MISS can address several spine conditions, including:

DISC offers various Ultra-MISS procedures depending on your specific condition. We will work with you to determine the best technique from the following:
A procedure that treats and removes herniated discs and spinal stenosis within the low back.
A surgery that treats chronic low back pain and facet joint syndrome, selectively severing problem nerves.
This technique decompresses painful nerves, treating foraminal stenosis that causes sciatica due to boney overgrowth of the facet joints.
This procedure targets the basivertebral nerve to treat vertebrogenic low back pain.
These outpatient procedures stabilize vertebral compression fractures in the spine.
Ultra-MISS uses various techniques to reach different areas of the spine. The expert surgeons at DISC are highly trained in these advanced procedures.
Patients are sedated with IV medication, and their skin surgical site is locally numbed. Patients are comfortable and responsive throughout the surgery. The surgeon then guides a spinal needle under fluoroscopic X-ray to the spinal disc (discectomy) or transverse process bone (medial branch transection/rhizotomy). A guidewire is inserted inside the needle, and the needle is removed. A 1/4-inch incision and a metal dilator are placed over the guidewire down to the disc, gently spreading the muscles. Next, a metal operating cannula is placed over the dilator, and the guidewire and dilator are removed, establishing a working portal. The surgeon then inserts an HD endoscope with a camera attached through the working cannula. Specialized micro-instruments are placed through the endoscope to assist the surgeon in ablating and decompressing the painful spinal nerves. The surgeon targets herniated discs and bone spurs that may impinge on a spinal nerve. After the surgery, the patient recovers for about an hour before going home. Because general anesthesia is not needed, the patient risk is significantly reduced and speeds up recovery time. Patients rarely require strong narcotic opioid medications after surgery.
Each of these ultra-minimally invasive procedures targets back pain resulting from a painful vertebra in the spine. Patients are sedated with IV medication, and their skin surgical site is locally numbed. Patients are comfortable and responsive throughout the surgery. Under fluoroscopic X-ray guidance, a physician directs an introducer cannula through the pedicle to the middle of the affected vertebra. In the case of Intracept®, a radiofrequency probe is inserted through the cannula to ablate the painful basivertebral nerve. With kyphoplasty and vertebroplasty, cement is injected through the cannula to stabilize a painful vertebral fracture. After the procedure is completed, patients recover for about an hour before going home.
As the Ultra-minimally invasive spine surgery leader, DISC surgeons are bridging the gap between pain management and major spine surgery. These procedures have excellent results in treating low back pain, leg pain and neck pain.
The following examples may be good candidates for ultra-minimally invasive spine surgery:



One of the key differentiating factors between ultra-minimally invasive and minimally invasive spine surgery is post-operative recovery and return to an active lifestyle. Ultra-MISS allows patients to return to administrative work as early as two to four days and physical work or play as early as four weeks.
Post-operative pain from Ultra-MISS can be easily managed with short-term narcotics and ibuprofen. In general, your recovery time can vary depending on your age and lifestyle practices.

After surgery, patients should not hesitate to call the office if they are experiencing any of the following conditions:
Any pain experienced worse than when you first left the surgery center should be communicated to the doctor’s assistant.
The sensation of “pins and needles” in the legs may be a sign of nerve damage due to spine surgery. If the feeling does not subside, contact your doctor’s office.
If either is experienced, contact your doctor immediately. Although not a common complication after surgery, it can be severe and should be reported immediately to your surgeon.
It is not uncommon for the surgical wound to cause pain within the first few days following surgery. If the pain increases, the wound gets red and puffy or has excessive drainage, this is a potential warning sign. Have a surgeon examine it to be safe.
Fever can be accompanied by chills and shaking.
This could be a sign of a blood clot. The pain will probably be mainly in the calf or thigh. The area may be tender and red to the touch. Blood clots can be a severe and life-threatening problem if they travel to the lungs or brain. Call your surgeon immediately.
DISC exists to bring expert minimally invasive spine surgery to patients across the world. We are passionate about providing compassionate care for patients experiencing painful spine conditions. You can trust us because:
As ultra-minimally invasive spine surgery leaders bridging the gap between pain management and major spine surgery, DISC provides procedures that have excellent results in treating low back pain, leg pain and neck pain. Contact DISC today to see if you may be a good candidate for ultra-minimally invasive spine surgery.
Our spine health blog features up-to-date spine education and expert spine tips from our spine specialists here at DISC.
1635 East Myrtle Avenue Suite 100, Phoenix, AZ 85020, USA
18700 North 64th Drive Suite 105, Glendale, AZ 85308, USA
8630 East Vía de Ventura Suite 210, Scottsdale, AZ 85258, USA
3487 South Mercy Road, Gilbert, AZ 85297, USA
1635 East Myrtle Avenue Suite 400, Phoenix, AZ 85020, USA